View File
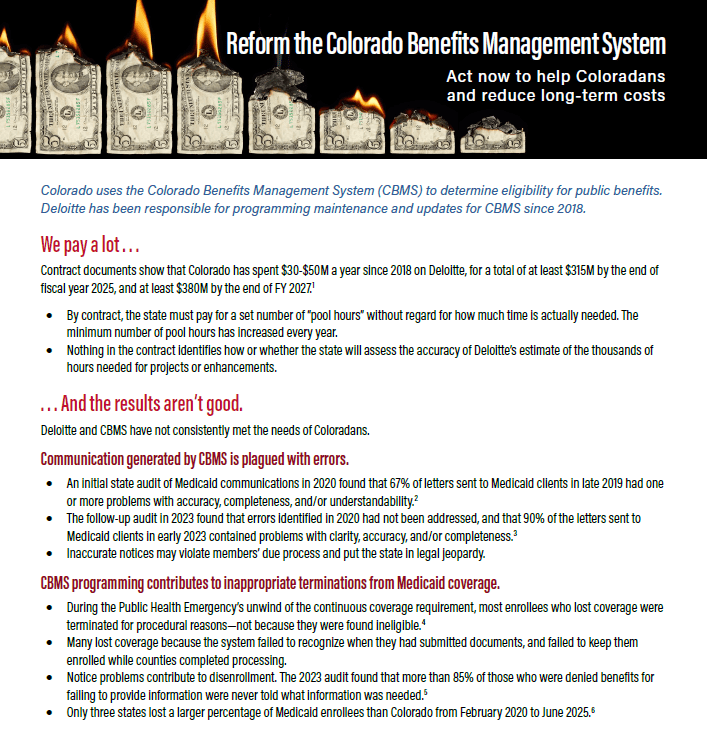
Churn is the word commonly used to describe the movement of people between public and private health insurance and between insured and uninsured status due to fluctuations in income and household size. Churn deserves considerable attention because of the potential adverse personal, administrative and financial impacts of frequent movement in and out of coverage. These impacts extend to individuals, families, health providers, insurance carriers and government health insurance programs.
While the Affordable Care Act (ACA) has made it possible for most people to enroll in health insurance, the potential for gaps in coverage remains significant. Estimates are that as many as fifty percent of adults below 200 percent of the Federal Poverty Level (FPL) will move between Medicaid and eligibility for subsidized private insurance through an Exchange at least once over the course of a year. Certain populations are more vulnerable to churn. For example, Colorado’s relatively high percentage of seasonal and self-employed workers are more likely to experience fluctuations in income over the course of a year, which may lead to changes in eligibility for insurance programs.
Many individuals who lose Medicaid will qualify for Advanced Premium Tax Credits (APTCs), through Colorado’s insurance marketplace, Connect for Health Colorado (C4HCO). APTCs are available to people with incomes under 400 percent of FPL and are designed to make private health insurance more affordable by offsetting the cost of premiums. However, while APTCs make it possible for people losing Medicaid to afford health insurance, transitions between Medicaid and tax credit eligibility present significant challenges. These challenges include finding and applying for new sources of coverage, navigating potential disruptions in care, managing changes in cost sharing obligations and overcoming administrative barriers to the application process. Additionally, gaps in coverage resulting from churn can lead to poorer health outcomes and increase costs for individuals and the health care system. Studies have found that “even brief interruptions in Medicaid coverage can lead to significant increases in hospitalizations for chronic diseases like diabetes, asthma and mental disorders.” While Colorado has taken significant steps to minimize the effects of churn, there is much more to do.

CCLP Public Comment to HHS Reinterpretation of Federal Public Benefit
Public Comment, Publications