Colorado health advocates presented to the Joint Budget Committee on glitch-plagued Public Health Emergency Unwind.
Recent articles
2024 Legislative session: addressing economic challenges at the individual and state level
Addressing economic challenges at the individual and state level after the 2024 Colorado legislative session.
CCLP’s 2024 legislative wrap-up, part 2
CCLP's 2024 legislative wrap-up focused on expanding access to justice, removing administrative burden, supporting progressive tax and wage policies, preserving affordable communities, and reducing health care costs. Part 2/2.
CCLP’s 2024 legislative wrap-up, part 1
CCLP's 2024 legislative wrap-up focused on expanding access to justice, removing administrative burden, supporting progressive tax and wage policies, preserving affordable communities, and reducing health care costs.
The true cost of Colorado’s unaccountably high Medicaid disenrollment rates
Millions of people who relied on Medicaid during the Public Health Emergency (PHE) are now navigating renewal processes around the country. Amidst the PHE unwind, thousands of individuals and families on Medicaid and CHP+ have received notices informing them that their healthcare coverage is ending. Though the end of the PHE has resulted in increased rates of disenrollment for people across the country, Colorado’s terminations are disproportionately high, creating a crisis for those who depend on these programs for healthcare coverage.
In Colorado alone, six months into the PHE unwind, 412,102 beneficiaries have been terminated from these programs. An alarming two-thirds of these terminations are for what are termed “procedural reasons.” In other words, just one-third of the terminations have been the result of a determination that the person or family is no longer eligible for the program (for example, because the person’s income exceeds limits, or because they no longer qualify as disabled, or perhaps because they have moved out of state.)
Though Colorado is in the middle of the pack in terms of state population (ranked 21st nationally), it is near the bottom in terms of rate of procedural disenrollments — only 9 states have higher rates than Colorado, and our net loss of members ranks Colorado an astounding seventh in the nation.[1]
The administration has largely dismissed concerns about the high rate of procedural disenrollments, though these rates are anything but normal. Both before the PHE and during the unwind, Colorado has had extraordinarily high rates of procedural disenrollments. This is the result of the fallout from a glitchy IT system, chronically flawed communications, problems with contractor and county oversight, and our fragmented, county-administered system. Penny-wise and pound-foolish, the state has been slow to invest in wholesale changes and the most vulnerable Coloradans are paying the price.
When people who should have stayed on Medicaid are instead kicked off the program, they have three routes back to coverage. Typically, fewer than a thousand Coloradans have appeal hearings each year, where they can ask an administrative judge to reinstate coverage or services. Others provide missing information to the county or wait out county processing delays while uninsured and hope to be redetermined eligible.
But based on CCLP’s review of data provided to the Centers for Medicare and Medicaid Services, a great many simply reapply. Our conversations with eligibility enrollment sites and community advocates support that interpretation, that many who lose coverage and feel certain they are still eligible will fill out a new application, rather than trying to get through to their county or face an appeal without representation.
A quick comparison shows the dire state of our state. Consider Maryland and Minnesota, two states whose state and Medicaid populations are very similar to Colorado’s. Maryland and Minnesota’s application rates were fairly constant before, during and after the PHE, while Colorado’s were much higher before the continuous eligibility requirements were put into effect for the PHE, and soared again immediately after the unwind began. For some months, Colorado’s numbers totaled more than six times as many applications as Maryland’s and Minnesota’s.
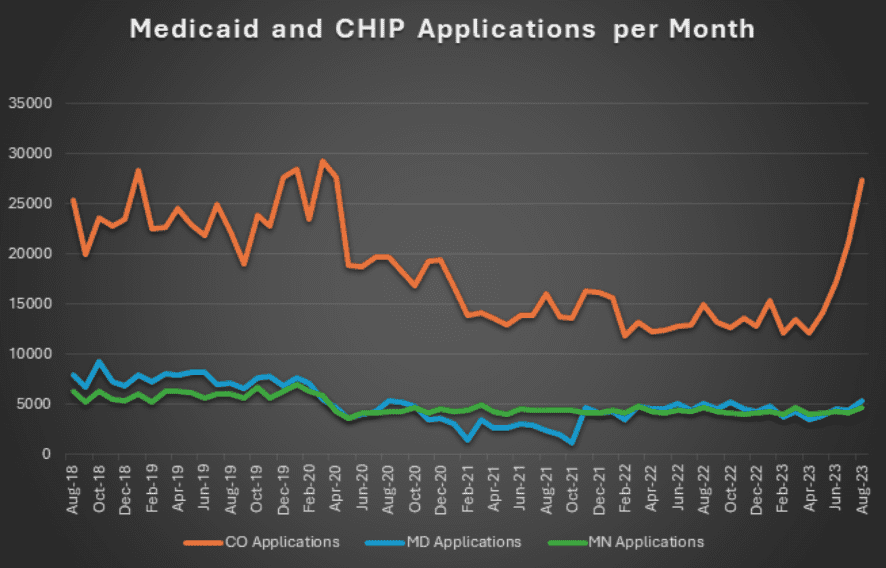
That Sisyphean loop of losing Medicaid and reenrolling is costly for counties and the state, and takes a real toll in terms of time, lost work, and stress for Medicaid members. Federal sources cite a 2015 estimate that states spend $400 to $600 dollars for each termination and re-enrollment. At that rate, 10,000 unnecessary applications per month would cost Colorado $4-6 million dollars a month, year in and year out.
The human cost is harder to calculate, but includes hours spent on the phone, waiting in county offices, gathering and uploading information, and the anxiety of not understanding where you’re going to get your next prescription or whether your scheduled surgery can take place as planned.
It doesn’t have to be this way.
In the short term, Colorado has the ability to put terminations for particular groups or larger populations on hold while the state digs into what is causing these outsized losses of coverage. That flexibility is available under special federal authority, along with other options to streamline renewals for people who utilize long-term services and supports. This would maintain coverage for vulnerable Coloradans and allow counties more time to keep up with the flood of renewals and new applications during the unwind. As we wait for longer term investments of resources in technology and enrollment assistance, it’s time to take that step to protect those that need it.
******
[1] Medicaid Enrollment and Unwinding Tracker, KFF, published Dec 13, 2023.

