CCLP presented our fourth Policy Forum event discussing tax credits in Colorado.
Recent articles
NHeLP and CCLP file for expedited review of civil rights violations in Colorado
On Sept 16, NHeLP and CCLP submitted a complaint to the Office for Civil Rights in the U.S. Department of Health and Human Services, addressing the ongoing discriminatory provision of case management services for individuals with disabilities in Colorado.
CCLP’s 26th birthday party recap
CCLP celebrated our 26th birthday party while reflecting on another year of successes on behalf of Coloradans experiencing poverty.
Small business displacement and Business Navigators
CCLP partnered with the city and county of Denver to administer a two-year program connecting Denver’s historically underinvested businesses with guides to programs, resources, and services available to them.
A first look at the Medicaid unwind: August 2023

Katie Wallat, CCLP’s Senior Attorney, provided testimony at the August 11, 2023, meeting of the Medical Services Board.
Good morning Mr. President and members of the board,
My name is Katie Wallat and I’m an attorney at the Colorado Center on Law and Policy, a statewide anti-poverty nonprofit organization. I wanted to take a quick moment this morning to provide additional perspective on how the Medicaid unwind process is going.
The Department has shared data on the first two months of the unwind process in public meetings, online, and to this board. This point-in-time data is often presented in comparison with what happened before the pandemic. However, while the pre-pandemic data provides a baseline, the state’s processing problems before 2020 were such that this is not a goal we think the department should be shooting for. The reported average rate of disenrollments for 2018-2019 was 40%, which is very high. We know that our Medicaid rolls did not dwindle by 40% each year before the pandemic, so many of these people must have been re-enrolled. This means that a large portion may have been terminated inappropriately or could not navigate the process of remaining enrolled. We know that we all have a shared goal of making sure this happens as little as possible.
I’d like to revisit the data for the past two months of renewals—by the end of June, a staggering 112,792 people have been disenrolled from Medicaid, which represents 45.7% of all of the people who were up for renewal. We know from our conversations in the community that this number includes not just those in the income-based categories, but many people with disabilities who rely on daily services to remain at home and in the community.
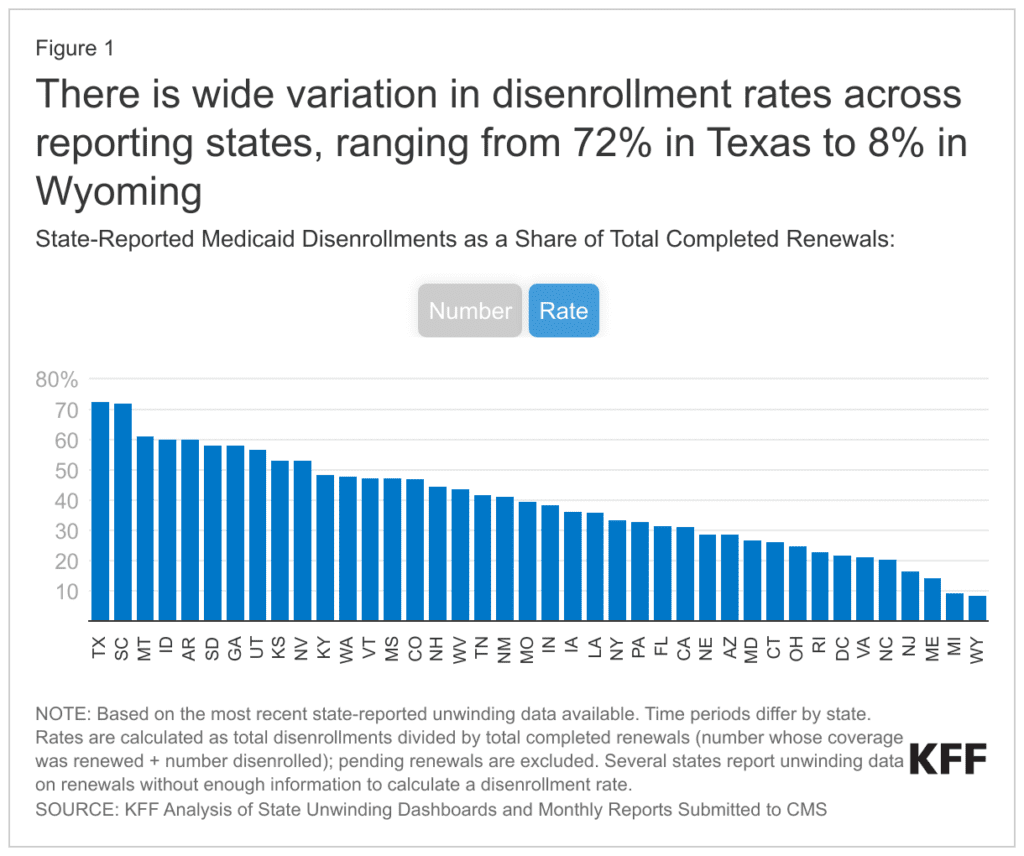
Unfortunately, Colorado is not doing very well relative to other states so far. A nonpartisan, independent source of health policy research called KFF, formerly the Kaiser Family Foundation, has been tracking each state’s reported data and providing comparisons. Colorado has the 15th highest rate of disenrollments in the nation. So, 35 other states, plus the District of Columbia, have had a lower rate of disenrollments during these first two months of the unwind.
Another important data point is the rate of what are called procedural disenrollments, which are distinct from disenrollments for an eligibility reason, where the state has sufficient information to determine that the person is ineligible. Procedural disenrollments, on the other hand, are those where the state terminates enrollment because it lacks sufficient information—either because they didn’t get a renewal packet back or information was missing—or because the county was unable to process the information received by the deadline. We have heard that many counties are currently overwhelmed with a backlog of applications and renewal packets.
In May alone, 50,253 people were disenrolled from Medicaid. The data from the Department show that 62% of them, or 31,000, were disenrolled for procedural reasons. In June, nearly half of the people who were up for renewal, or 62,539 people, were disenrolled. Of these, nearly 44,000, or 70% of them, were disenrolled for procedural reasons. We’re not drawing conclusions about trends from just two months of data, but we are frankly distressed about what this means for the 75,000 Coloradans with procedural denials over just the first two months of the unwind process. The Centers for Medicare and Medicaid Services has also expressed concerns about that rate in a letter to the state that was publicly posted yesterday.
CCLP is among the community organizations that have been contacted on a near-daily basis by families who have been disenrolled. I want to paint a picture of some of these individuals that the data are describing.
Thanks to the outreach that the department and case management agencies have undertaken to spread the word about the unwind, one family we’re in contact with was aware of the upcoming need to fill out the renewal paperwork for their disabled child, but report that they never received a renewal packet in the mail. Instead, the family went to the county office in person, to fill out their packet before their renewal deadline. Despite their vigilance, the paperwork was not processed in time by the county and the child’s Medicaid was terminated. As a result, the family was unable to get the G-tube supplies needed and had to pause therapy appointments until the child was reinstated. According to the data, this person would have been considered one of the people who were procedurally disenrolled because of a failure to complete the renewal packet.
Another child has been on Medicaid for 8 years. The parents also reported not receiving a renewal packet, but they did receive a letter asking for additional information. She submitted that information before the deadline and confirmed by phone with the county that it had been received. But because the information was not processed in time, her child was disenrolled from Medicaid, for the procedural reason of “failing to provide verification.” A major surgery had to be put on hold because of this.
More terminations are pending, and advocates are scrambling to prevent them from taking place. One parent has learned that her infant, born prematurely and dependent on oxygen, will lose Medicaid at the end of the month. She has been told that the county will be unable to process his application before the renewal deadline—meaning that he, too, will be counted among those who “failed to complete the renewal process” when data is tabulated, unless advocates can help her stop that from happening.
I could share a dozen more stories, and other community members could as well. Our goal in sharing these stories is to give a more nuanced perspective of what these categories can and do mean for real families. We recognize how hard the Department is working to conduct what can only be described as a herculean task, which is complicated by having to work with eligibility staff in 64 different counties.
HCPF has been responsive to resolve individual cases that we and others bring to them. But for every case we hear of, we know there are many times as many people terminated in the last three months who don’t know who to call. We have had promising conversations with the Department about working together to fix some of these problems but want to emphasize that fixing these issues may call for fundamental changes to how eligibility applications are processed. We know that good communication channels, hands-on assistance with renewal packets, and timely processing can help keep procedural disenrollments to a minimum. We thank the Department for their ongoing partnership and will continue to share information with this board, as the unwind continues. Thank you for your time and attention.
Sincerely,
Katherine Wallat
Senior Attorney
Colorado Center on Law and Policy
