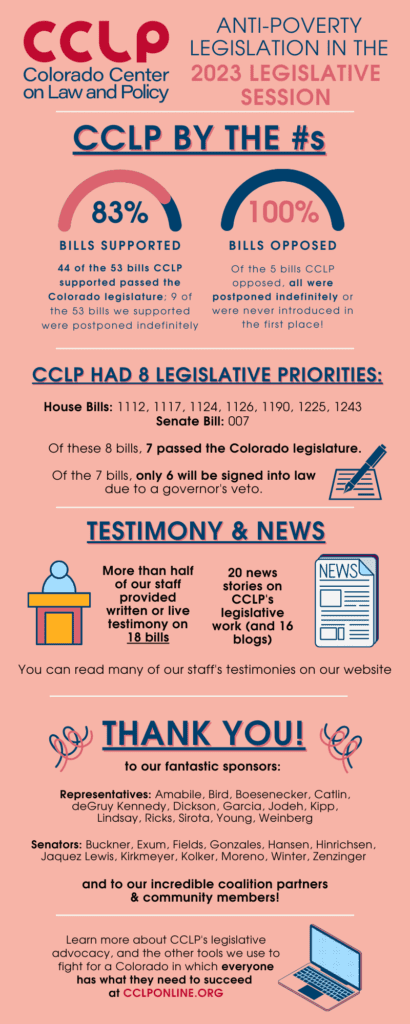
A summary of the list of recommendations on the implementation of the OBBBA in Colorado regarding public benefits systems and work requirements.
Recent articles
CCLP testifies in support of Colorado’s AI Sunshine Act
Charles Brennan provided testimony in support of Senate Bill 25B-004, Increase Transparency for Algorithmic Systems, during the 2025 Special Session. CCLP is in support of SB25B-004.
Coloradans launch 2026 ballot push for graduated state income tax
New ballot measure proposals would cut taxes for 98 percent of Coloradans, raise revenue to address budget crisis.
CCLP statement on the executive order and Colorado’s endless budget catastrophe
Coloradans deserve better than the artificial budget crisis that led to today's crippling cuts by Governor Jared Polis.
2023 Legislative Review, Part 2: Medical Debt and Health Care
The high cost of health care leaves too many Coloradans with bills they cannot afford to pay — and can even deter people from seeking needed medical care in the first place. One in eight Coloradans have medical debt in collections[i], and low-income people and communities of color are disproportionately impacted.
In previous years, CCLP led groundbreaking legislation to reform the hospital bill collections process, HB21-1198. This law requires all Colorado hospitals to provide low-income hospital patients with discounts and affordable payment plans, among other patient protections. (Learn more about Colorado’s new Hospital Discounted Care law at cohealth.co/hospitaldiscounts.)
This year, five bills – including one of CCLP’s priority bills – addressed medical bills and medical debt. CCLP led efforts on HB23-1126, which stops medical debt from being included on credit reports, except in very limited circumstances. Bad credit reports not only hurt one’s ability to qualify for affordable credit, but they can also affect access to rental housing, employment, insurance, and more. The State Attorney General’s Office led the effort of SB23-093, which strengthens consumer protections in the medical billing and collections processes, including limiting interest on medical debt to 3%.
A hospital Medical Price Transparency bill, SB23-252, continues to build on federal legislation which requires hospitals to give online pricing information for consumers to compare treatment costs between hospitals prior to treatment and incurring costs. CCLP supported previous state legislation, HB22-1285, which prohibited certain debt collection practices if the hospital was not in compliance with price transparency requirements. State law will require hospitals to include costs, negotiated rates, and discounted cash prices.
New solutions for rising costs
Colorado Consumer Health Initiative also led a coalition which included CCLP in limiting Hospital Facility fees, HB23-1215. Many Coloradans are surprised to get a medical bill with an unexpected facility fee, which can be hundreds or even thousands of dollars and is frequently not covered by insurance. Strongly opposed by the Colorado Hospital Association, the bill was narrowed, but passed as a prohibition of facility fees on outpatient preventative care, a requirement to disclose and post the fee, to list the fee separately on the bill, and for Colorado Department of Health Care Policy & Financing (HCPF) to produce a report on the impact of facilities fees in Colorado.
Another contributor to high medical costs can be the high cost of certain prescription drugs. While many contribute greatly to maintaining health and fighting disease, and may reduce potential costs of hospitalizations, many critical drugs are priced excessively. CCLP advocated for the creation of The Prescription Drug Affordability Review Board with SB21-175. It authorized the board to review up to 12 drugs to assess price and to establish upper payment limits on them. With this year’s HB23-1225 the 12-drug limit was removed, in large part because one drug can have multiple versions.
Another major update to HB19-1320, which was originated by CCLP, was the community benefit for non-profit hospitals. Taxpayers invest hundreds of millions of dollars in Colorado nonprofit hospitals through tax exemptions. Nonprofit hospitals receive these very substantial financial benefits on the condition that they invest in services and activities to help improve health outcomes in the communities they serve. HB23-1243, Hospital Community Benefit, strengthens the hospitals’ reporting requirements, HCPF’s enforcement mechanisms, and, most importantly, the process by which communities are engaged to have a voice in determining how these investments are spent. Strengthening the community engagement aspect of these investments is one way of ensuring that there is a direct connection between the significant and wide-ranging needs in our communities, and the investments that hospitals provide.
Protecting access for Coloradans
This session, CCLP supported two important bills regarding access to health care. HB23-1300, led by Colorado Children’s Campaign, directs HCPF to conduct a study of continuous medical coverage by January 1, 2026, including preparing documents needed to seek authorization from the federal government. In addition, by April 1, 2024, HCPF is required to seek federal authorization to provide continuous coverage for Colorado children under 3 years of age, regardless of immigration status. HCPF would also seek authorization for 12 months of coverage for adults being released from the state’s Department of Corrections facilities.
CCLP researched and advocated for including these provisions. CCLP also testified in favor of a Division of Insurance bill as a voice for consumers, HB23-1303, which would protect Coloradans from insolvent insurers. Currently, two Colorado Health Maintenance Organizations (HMOs) have been on the brink of insolvency which would have had ripple effects across the industry. HB23-1303 would require all HMOs in Colorado to contribute to the fund to insure their solvency.
Another success from this year included a Reproductive Rights package in the form of SB23-188, SB23-189, SB23-190. Since the passage of these bills in mid-April, Colorado has become a haven for abortion care. The package further expanded protections around reproductive health care for patients and providers, including gender-affirming care for transgendered people; increased access to reproductive health care by requiring certain health insurance carriers to cover this type of care; and ended deceptive trade practices in pregnancy-related services, such as collusive marketing and advertisements by “faux”/crisis pregnancy clinics. By signing these bills into law, Colorado continues to protect the rights of individuals to choose what is best for their own body.
Immigrant access to public benefits
Last summer, CCLP brought to the attention of the CDHS and HCPF that Colorado’s prohibition on beneficiaries sponsoring family members or other individuals to immigrate to the U.S. was in violation of federal law. The state agencies agreed, and CDHS introduced HB23-1117, Affidavit of Support Eligibility Public Benefits. CCLP supported the bill, which passed and was signed into law, making the state compliant with the federal statute.
Behavioral health
The weight, pain, and damage of mental health difficulties are affecting a growing number of Coloradans and their families. Access to services is limited by the increased need for such services, a workforce that is burned out, and broken internal systems. CCLP supported SB23-174, Expanding Access to Behavioral Health Services for Colorado Kids, which removes the prerequisite of needing a formal behavioral health diagnosis for behavioral health services. This bill opens access to a wide array of services, such as psychotherapy and services related to case management, prevention, education, and outreach. This policy applies to thousands of kids across the state covered by Medicaid and the School Health Services Program. By eliminating the diagnosis requirement more Colorado kids and their families can access affordable, early, prevention-focused services before a crisis occurs.
HB23-1007, Higher Education Crisis and Suicide Prevention bill requires crisis and suicide prevention numbers to be printed on student ids for higher education students. This simple action could provide convenient information and a lifeline at the right time while in a mental health crisis.
The criminal justice system, prisons, and jail are too often the mental health providers of first resort. This has been long known and bemoaned. HB23-1153 requires research on the feasibility of creating a system to support individuals with serious mental health illness through a collaboration between Colorado’s behavioral health and judicial systems.
As we like to point out at CCLP, the passage of a bill into law is only the beginning, but not the end of the work that needs to be done. Rulemaking and public input opportunities, outreach and public information, and implementation are the steps which help these policies take form, giving them the power to better the lives of Coloradans experiencing poverty. Even as that timeline plays out this year, work has already begun through our various organizational partnerships and coalitions on our 2024 legislative agenda.
[i] https://kdvr.com/news/data/study-1-in-8-coloradans-is-in-medical-debt/
